Study links disrupted brain fluid flow to poorer survival in glioblastoma patients
For decades, doctors have focused on the size, location, and behavior of glioblastoma tumors to gauge how patients might fare. But new research suggests that the brain’s internal fluid-circulation network may hold equally important clues about survival in the most common form of the disease.
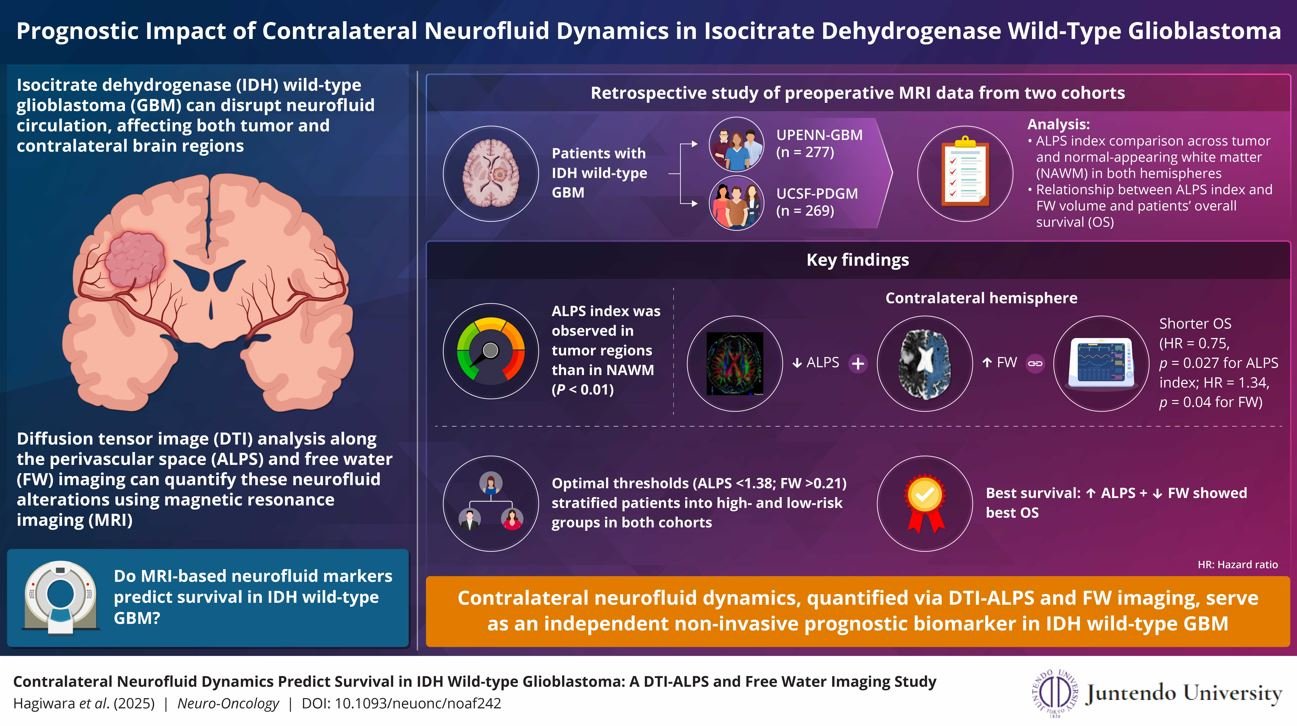
A team of scientists from Juntendo University reported that patients with IDH wild-type glioblastoma showed major differences in survival depending on how well their brains cleared fluid, even in regions untouched by the tumor. The findings point to a hidden layer of disease progression that traditional imaging often fails to show.
Published on Oct. 11, 2025 in Neuro-Oncology, the study analyzed MRI scans from 546 patients across two clinical datasets. Using sophisticated imaging markers, the researchers evaluated fluid movement within the contralateral hemisphere, the side of the brain opposite the tumor, where no visible abnormalities typically appear.
Impaired fluid flow emerges as a powerful survival marker
The investigators relied on two MRI indicators: the DTI-ALPS index, which measures the ease of water movement along perivascular channels, and free water imaging, which detects fluid buildup between brain cells. Lower ALPS values and increased free water strongly correlated with shorter survival, regardless of tumor burden.
Lead researcher Akifumi Hagiwara said the discovery shows that glioblastoma disrupts the brain far more broadly than once assumed. Even distant areas, he explained, can develop signs of slowed clearance and hidden toxicity that influence how patients respond to treatment.
These disruptions involve the glymphatic system, the brain’s fluid-drainage network responsible for removing metabolic waste and inflammatory byproducts. When this system falters, the environment surrounding brain tissue becomes increasingly unstable, potentially accelerating the disease process.
A potential shift toward personalized treatment strategies
Patients in the study with healthier glymphatic activity survived significantly longer than those with impaired flow, suggesting that neurofluid dynamics might become an important biomarker for risk assessment. If validated clinically, doctors could use these MRI patterns to tailor treatment intensity or identify candidates for emerging therapies.
Researchers also believe the insights could spark new treatment directions. Approaches that improve glymphatic function—such as regulating sleep cycles, reducing inflammation, or altering water-channel activity—may eventually complement surgery, radiation, and chemotherapy.
Hagiwara emphasized that the work challenges long-held assumptions about glioblastoma as a disease confined to a single mass. Instead, he said, the cancer appears to disturb how the entire brain maintains its internal balance, making fluid-flow metrics a potentially crucial piece in understanding survival.
The study’s authors maintain that broader use of MRI-based fluid assessments may deepen understanding not only of glioblastoma but of other neurological disorders involving impaired waste clearance, including Alzheimer’s disease.



